Healthcare organizations operate in one of the most contract-heavy and heavily regulated sectors in the world. Obligations hidden within payer contracts, provider agreements, BAAs, clinical SLAs, medical device contracts, and cross-border regulations are frequently untracked or misunderstood. These gaps lead to revenue leakage, audit findings, regulatory exposure, and even patient-care risks.
The fix requires three things:
• Accurate and automated detection of all obligations
• Proper operationalization with ownership, workflows, and controls
• Continuous monitoring that evolves with regulatory and contract changes
Aavenir ComplianceNext operationalizes this end-to-end by centralizing obligations, automating workflows, and delivering real-time compliance visibility across the entire healthcare contract ecosystem.
Is your healthcare organization struggling with obligations buried across contracts?
Aavenir ComplianceNext offers unified visibility, automated workflows, and continuous monitoring to eliminate blind spots and strengthen compliance governance.
Healthcare Runs on Contracts, and Compliance Is Breaking
Healthcare contracts define everything from reimbursement to patient safety, but compliance workflows are not built to handle their complexity.
Healthcare is driven by thousands of interconnected contracts. Payer agreements determine reimbursements and penalties. Provider contracts govern credentialing, quality metrics, and service obligations. Vendor contracts define uptime, device maintenance, and data protection. BAAs specify how PHI must be handled. Clinical research agreements dictate safety oversight and reporting.
Yet despite large compliance teams and regulatory oversight, healthcare organizations still miss critical obligations. These gaps occur because healthcare contracts are long and complex, and are often stored across departments with no unified tracking system. As regulations like HIPAA, CMS rules, GDPR, MDR, and NHS procurement standards evolve, older contracts fall out of sync, creating compliance risks.
Understanding why compliance breaks are the first step toward fixing them.
Why Contract Compliance Breaks in Healthcare
Compliance fails because obligations are fragmented across documents, teams, systems, and outdated workflows.
Fragmented and Overlapping Contract Types
Healthcare deals with payer contracts, provider agreements, device and equipment contracts, BAAs, MSAs, and research agreements. Obligations span multiple teams, but no single owner sees the complete picture.
Regulatory Updates Outpace Contract Updates
Regulations from CMS, OIG, HIPAA, GDPR, NHS, and MDR change frequently. Legacy contracts remain outdated because updates require renegotiation, legal review, and new workflows.
Siloed Data Across Departments
Legal stores contracts. Compliance tracks checklists. Revenue cycle handles reimbursement. IT manages BAAs. Supply chain handles device vendor terms. No unified system connects them.
Manual Monitoring Workflows
Teams rely on spreadsheets, email reminders, and institutional knowledge. Compliance becomes reactive rather than proactive.
Institutional Memory Risk
Key obligations are often known only to certain individuals. When roles change, knowledge disappears, and gaps widen.
Where Contract Compliance Gaps Show Up: North America
In North America, gaps most often appear where payer rules, data privacy, and operational complexity intersect.
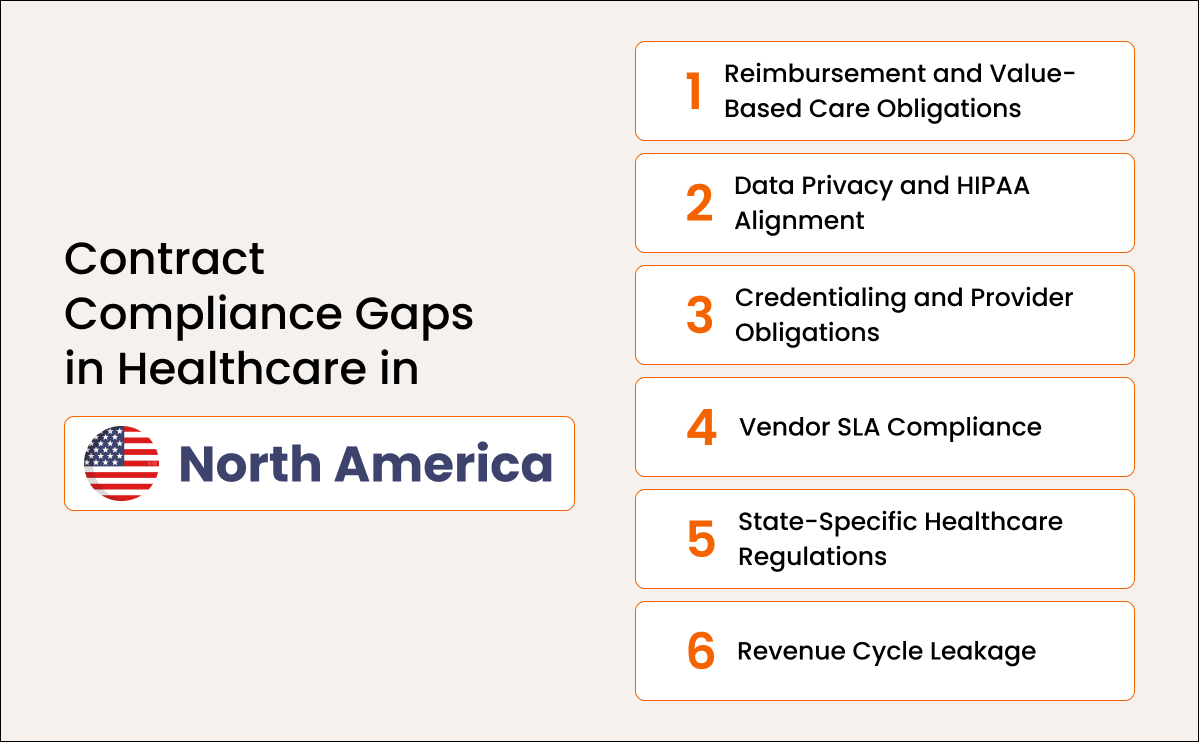
Reimbursement and Value-Based Care Obligations
CMS and commercial payer contracts include detailed quality metrics, reporting timelines, and reimbursement dependencies. Missing a single requirement results in payment denial or penalties.
Data Privacy and HIPAA Alignment
Missing BAAs, incomplete data-sharing clauses, and outdated PHI-handling terms create significant compliance risks.
Credentialing and Provider Obligations
Provider agreements require credentialing checks, privileging duties, and directory updates. Missed obligations lead to regulatory issues or claim denials.
Vendor SLA Compliance
Medical device companies, telehealth vendors, outsourced billing teams, and IT partners all have performance obligations that often go unmonitored.
State-Specific Healthcare Regulations
US states impose unique telehealth, privacy, reimbursement, and medical licensing rules that are often missing from enterprise templates.
Revenue Cycle Leakage
Obligations tied to claim submission deadlines, reimbursement structures, and prior authorization terms frequently go untracked, leading to preventable revenue loss.
Where Contract Compliance Gaps Show Up: Europe
Europe faces intense contractual complexity due to GDPR, MDR, NHS procurement frameworks, and cross-border healthcare laws.
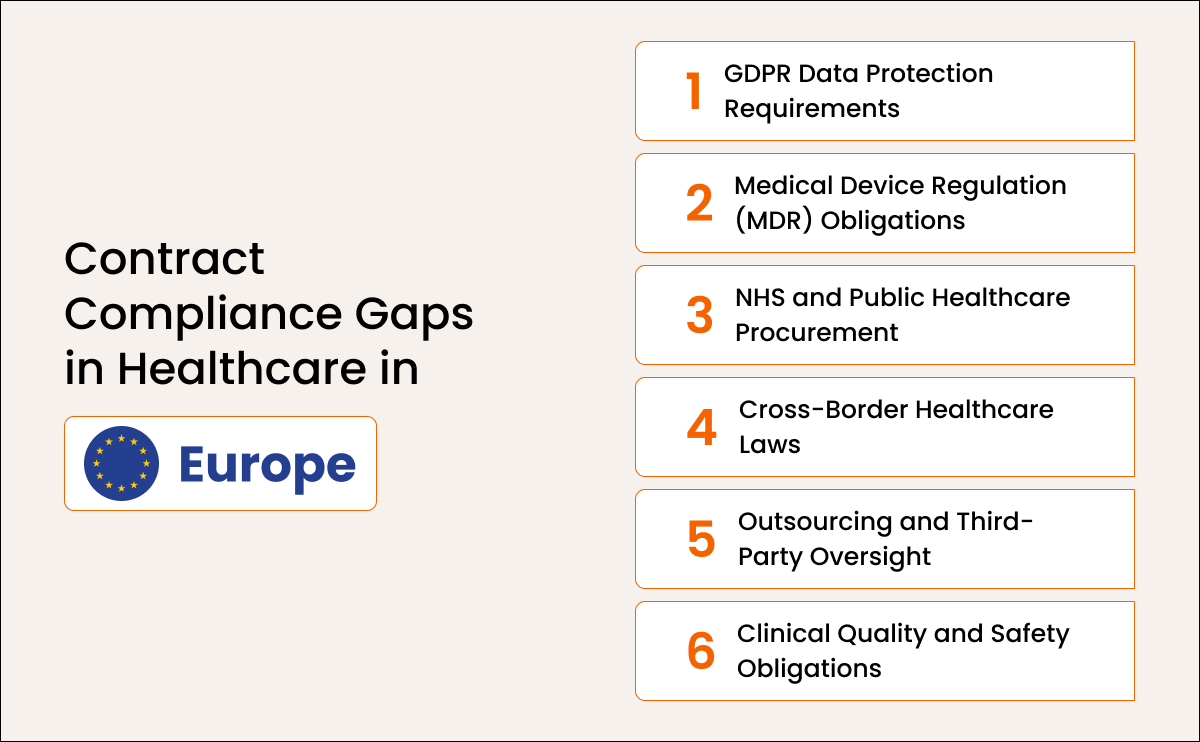
GDPR Data Protection Requirements
Healthcare contracts must define data responsibilities, processors, retention periods, breach notification timelines, and patient-rights handling. Missing terms create regulatory exposure.
Medical Device Regulation (MDR) Obligations
Contracts with device vendors often lack required safety documentation, maintenance evidence, or monitoring of corrective actions.
NHS and Public Healthcare Procurement
Public-sector agreements require strict adherence to SLAs, audit access, reporting, and performance measurements that are often unmonitored.
Cross-Border Healthcare Laws
Contract obligations involving EU, EEA, and UK entities are frequently inconsistent, leading to compliance conflicts.
Outsourcing and Third-Party Oversight
Healthcare systems often fail to enforce audit rights, SLA performance, or regulatory responsibilities with outsourced partners.
Clinical Quality and Safety Obligations
Performance standards, patient safety documentation, and clinical reporting often fall between operational and legal teams.
Why These Gaps Matter
Contract compliance gaps directly impact financial performance, regulatory exposure, and patient safety.
Revenue Leakage
Missed reimbursement terms, penalties for late reporting, and incomplete payer compliance can cost millions annually.
Regulatory Exposure
Violations of HIPAA, GDPR, CMS, NHS, MDR, or Joint Commission standards result in fines, investigations, and public scrutiny.
Patient Safety Risks
Missed device maintenance, unmonitored SLAs, or inadequate credentialing can directly endanger patient care.
Audit Disruption
Incomplete documentation slows internal audits, payer audits, and regulatory inspections.
Operational Inefficiencies
Teams lose time resolving issues that could have been prevented with proper obligation tracking.
How to Detect Compliance Failures Before They Escalate
You cannot fix compliance gaps unless you first surface every obligation across every agreement.
Centralize All Contracts
Bring payer agreements, BAAs, provider contracts, vendor MSAs, and device agreements into one system.
Extract Obligations and Classify Them
Turn complex legal text into structured obligations with categories, tags, and owners.
Compare Templates Against Executed Contracts
Detect missing clauses in HIPAA language, reimbursement terms, data protections, and device safety requirements.
Map Obligations to Owners and Teams
Assign responsibilities to revenue cycle, compliance, IT, clinical operations, or supply chain teams.
Reconcile Contracts With Operational Data
Check if payer obligations are reflected in EMR workflows, billing systems, or vendor dashboards.
Use AI for Large-Scale Detection
AI can rapidly detect missing clauses, inconsistencies, renewal triggers, SLA deviations, and regulatory mismatches.
Are obligations from contracts, agreements, and vendor SLAs getting missed?
Aavenir Obligationflow extracts, organizes, and operationalizes every obligation across complex healthcare contracts so teams always know what needs to be done and when.
How to Fix the Compliance Breakdown: A Framework for Healthcare
Fixing compliance is about operationalizing obligations, not just identifying them.
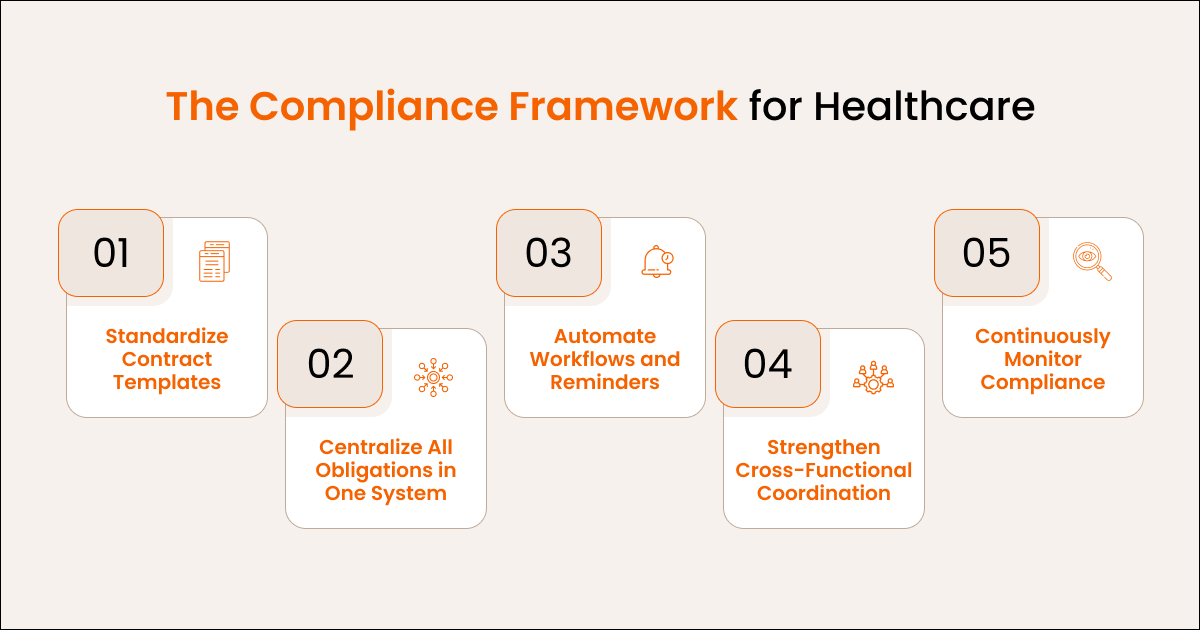
Standardize Contract Templates
Bring consistency to BAAs, payer contracts, vendor agreements, and device SLAs.
Centralize All Obligations in One System
Give teams a unified source of truth that eliminates the need for scattered tracking methods.
Automate Workflows and Reminders
Ensure deadlines, reporting tasks, and renewal actions are completed on time.
Strengthen Cross-Functional Coordination
Clinical ops, legal, revenue cycle, IT, compliance, and supply chain must work from the same obligation set.
Continuously Monitor Compliance
Assign owners, track evidence, escalate issues, and show regulators complete audit trails.
The Operational Answer: How Aavenir ComplianceNext Solves the Problem
Healthcare compliance demands automation and unified visibility that manual systems cannot provide. Aavenir ComplianceNext is an AI-driven compliance engine that identifies contractual obligations, maps them to regulatory frameworks, and automates execution with alerts, workflows, and audit-ready evidence.
ComplianceNext offers:
- • Unified obligation extraction from all healthcare contract types
- Mapping to HIPAA, CMS, GDPR, MDR, and NHS frameworks
- Automated workflows with deadlines, owners, and documentation
- Real-time monitoring of SLAs, reimbursements, data protections, and safety obligations
- Evidence capture for audits and regulatory reviews
- Scalability across multi-hospital systems and payer networks
Conclusion
Healthcare cannot afford compliance blind spots; the future belongs to systems that unify obligations, automate execution, and sustain continuous compliance.
Contracts will only grow more complex. Regulations will become stricter. Operational models will expand across telehealth, AI, cross-border care, and integrated delivery networks. The answer is building compliance around structured obligations, automation, and continuous monitoring.
With Aavenir ComplianceNext, healthcare organizations can finally eliminate compliance gaps and operate with clarity, control, and confidence.
Healthcare Compliance Needs More Than Manual Tracking
Healthcare compliance demands more than spreadsheets and reminders. ComplianceNext centralizes obligations and enforces accountability at every step.